1up Payer to Payer
Overview for payers partnered with 1upHealth
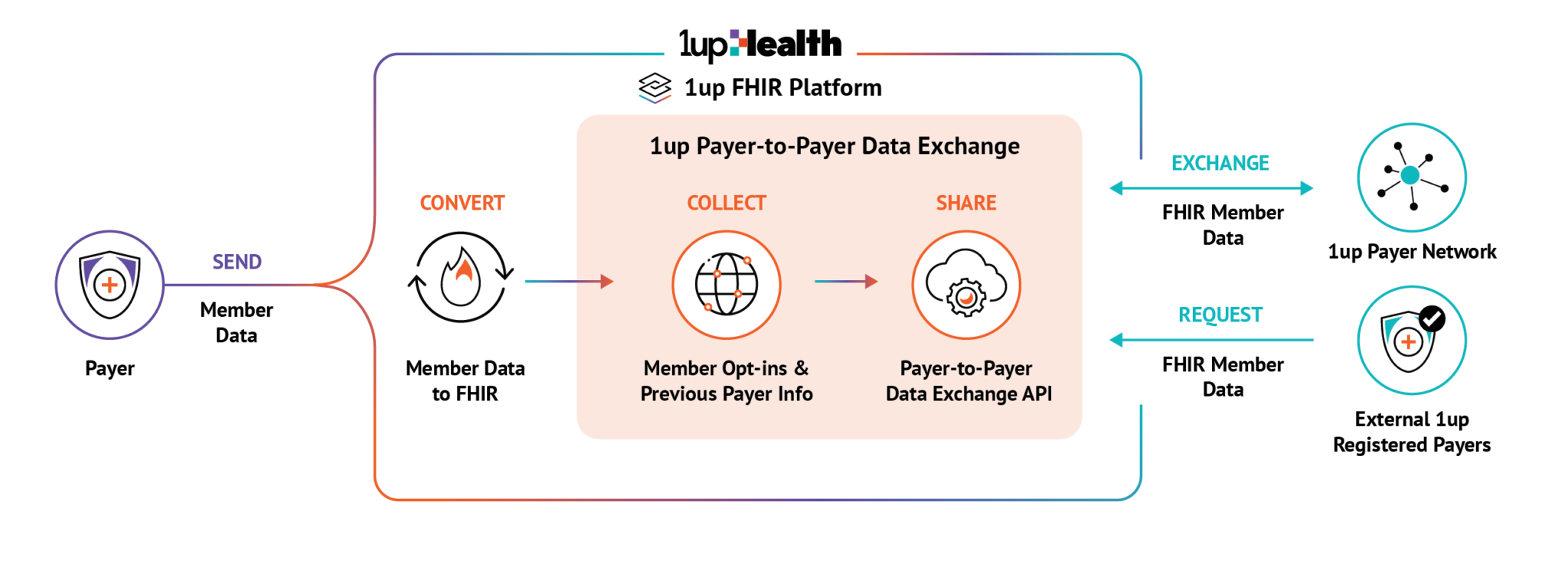
Designed to meet CMS Interoperability and Prior Authorization Final Rule (CMS-0057-F) requirements and leveraging industry standards, the 1up Payer-to-Payer Data Exchange API lets you easily and securely exchange member data with other payers in a standardized format—eliminating manual processes and administrative costs.
Our FHIR®-based API allows you to share and receive health data with other payers for new and previous members who have opted into data sharing, excluding cost-sharing and remittance dollar amounts. Incorporating data from other payers gives you a complete view of your member base and supports more informed and efficient decision-making.
Payers that are partnered with 1upHealth can use the templates provided under Member education to satisfy CMS's requirement for payers to provide plain language resources to members.
Overview for external payers
As a health plan who is not a 1up customer, you can make requests to 1up's Payer to Payer APIs to export data for members that have switched to your coverage, or have concurrent coverage with you.
Payer organizations can query 1upHealth to receive member data from our partnered payer organizations. Payers must register on the 1up Dev Portal and complete the identity verification process to query production data, but payers can perform test queries using a sandbox client before receiving access to production. For more information, see Payer implementation.
